Causes, Symptoms And Prevention Of Periimplantitis
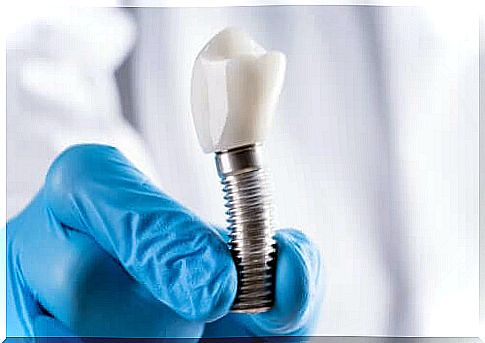
Currently, there are various solutions for replacing missing teeth, although some common ones, such as dental implants, can lead to periimplantitis. In fact, complications can occur even though they are mostly effective, aesthetically accurate, durable and safe.
This condition manifests itself as inflammation of the soft and hard tissue that surrounds an implant. It involves both the mucosa and the supporting tissue, leading to progressive destruction of the bone structure that holds the implant in place.
This article describes the causes and symptoms of this complication. In addition, we tell you how to treat it. Read on and find out more.
Causes of periimplantitis
Bone loss around the implant has a multifactorial origin. In addition, there are two main etiological causes of periimplantitis:
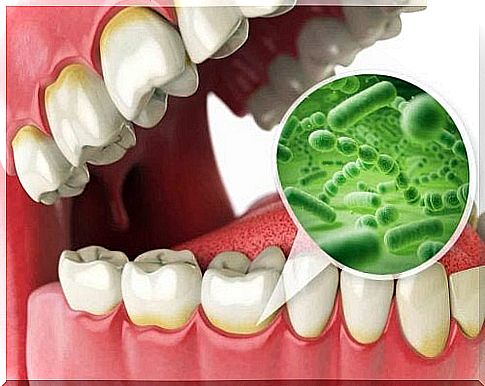
- Bacterial flora is the presence and accumulation of bacteria from the mouth on the implant surface.
- Occlusal overload is the biomechanical load generated during chewing movements that can lead to fracture and resorption of the peri-implant bone (this occurs when the implant placement is incorrect and the mechanical forces are not distributed in a balanced way).
Risk factors
As mentioned above, periimplantitis is due to bacterial colonization and occlusal overload of the implant. However, there are other factors that lead to this disease.
The patient’s habits, genetic conditions or the presence of any pathology may predispose a person to this condition. The dentist must consider these things before inserting the implant. Accurate diagnosis and evaluation of bones and gums before surgery is essential to prevent complications.
Some of the risk factors for periimplantitis are:
- Smoking.
- Poor quality of the supporting tissue.
- Periodontal disease and gingivitis.
- Systemic diseases: Among others osteoporosis, some cancers and diabetes.
- Poor oral hygiene.
- Bacterial contamination when the implant is inserted.
- Poor distribution of occlusal forces that generate overload.
- Stress.
What are the symptoms of periimplantitis?
These are similar to the symptoms of periodontal disease in natural teeth. As we said above, it is the inflammation in the tissues that surrounds and supports the implant.
There is bacterial plaque and tartar, swelling and redness of the mucous membranes around the implant. In addition , it can soften from the area by brushing, rubbing and during tooth cleaning.
Sometimes suppuration is also seen around the implant. Especially if the hole is larger than six millimeters (when the dentist performs a probe that measures the distance from the gums to the base of the sulcus).
They can also control the loss of bone tissue through X-rays. In fact, the mobility of the implant is a sign of the development of this condition. In addition, it is usually painless, but some patients experience discomfort when they bite their teeth together.
A person with these symptoms should consult a dentist immediately. This is because the sooner they deal with this complication, the better the prognosis.
In any case, regular check-ups after an implant are also important. Few people are aware of having this disease.
Diagnosis of periimplantitis
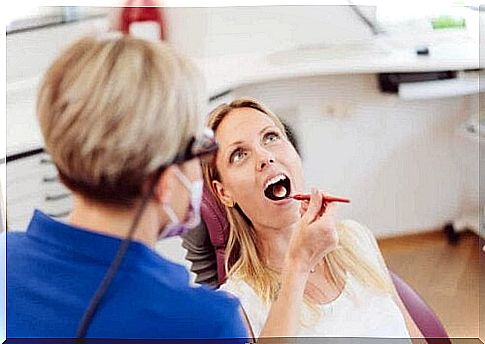
As we mentioned above, regular visits to the dentist for evaluation of the tissue around the implant and the levels of bacterial plaque in the mouth are basic. Thus, they can deal with it early to stop its progression as quickly as possible.
The diagnosis of the pathology focuses on detecting changes in soft tissue and in the bone around the implant. Clinical examination and measurement of depth allows evaluation of the presence of cavities, gingivitis, bleeding, suppuration and implant mobility.
X-rays are also needed. This is because they allow you to analyze the bone density and whether there is reabsorption around the device.
Treatment options for periimplantitis
Treatments for periimplantitis seek to control the infection to stop further damage and bone loss. The dentist must be able to choose the most appropriate treatment depending on the degree of the situation.
They can prescribe antibiotics to treat the infection, either orally or topically – by placing devices that release them into the hole.
In addition, they can perform subgingival debridement or scaling. This consists of separating the gum tissue manually to eliminate inflammation and promote its healing.
Surgical treatment will be necessary when periimplantitis has significantly damaged the bone. There are various techniques you can use to meet your specific needs:
- Access surgery consists of opening a flap to remove the damaged tissue, cleaning and disinfecting the implant surface.
- In resection surgery, the properties of the bone and soft tissue are modified to avoid the formation of new holes in addition to the above.
- Regenerative procedures consist of the placement of grafts or barrier membranes to restore the lost bone.
Adjustments to the prosthesis portion of the implant are also part of the treatment. It prevents occlusal congestion.
In addition, there is also improvement in the patient’s hygiene habits. The dentist should give instructions on the necessary measures to check the cleanliness of the mouth. In addition, the dentist may prescribe the use of antiseptic mouthwash, such as chlorhexidine, to reduce bacterial spread.
Taking care of the implant is essential
Some uncontrollable factors may give rise to periimplantitis. However, caring for an implant is fundamental to reducing the risk of complications.
Thus, oral hygiene is essential so that brushing at least twice a day and after each meal can prevent the accumulation of bacteria that can lead to problems with the implant.
Particular attention must also be paid to reaching the most inaccessible areas and cleaning all teeth in the mouth. Flossing and rinsing your mouth helps a lot.
Smoking significantly increases the risk of periimplantitis as this habit is related to mucositis and bone loss.
In case of bruxism due to stress, treatment and the use of splints are necessary to avoid occlusal overload on the implants.
As already mentioned, regular dental checkups are also important to detect any problems in a timely manner. The sooner a dentist makes a diagnosis and prescribes treatment, the better the prognosis for the implant in the mouth.